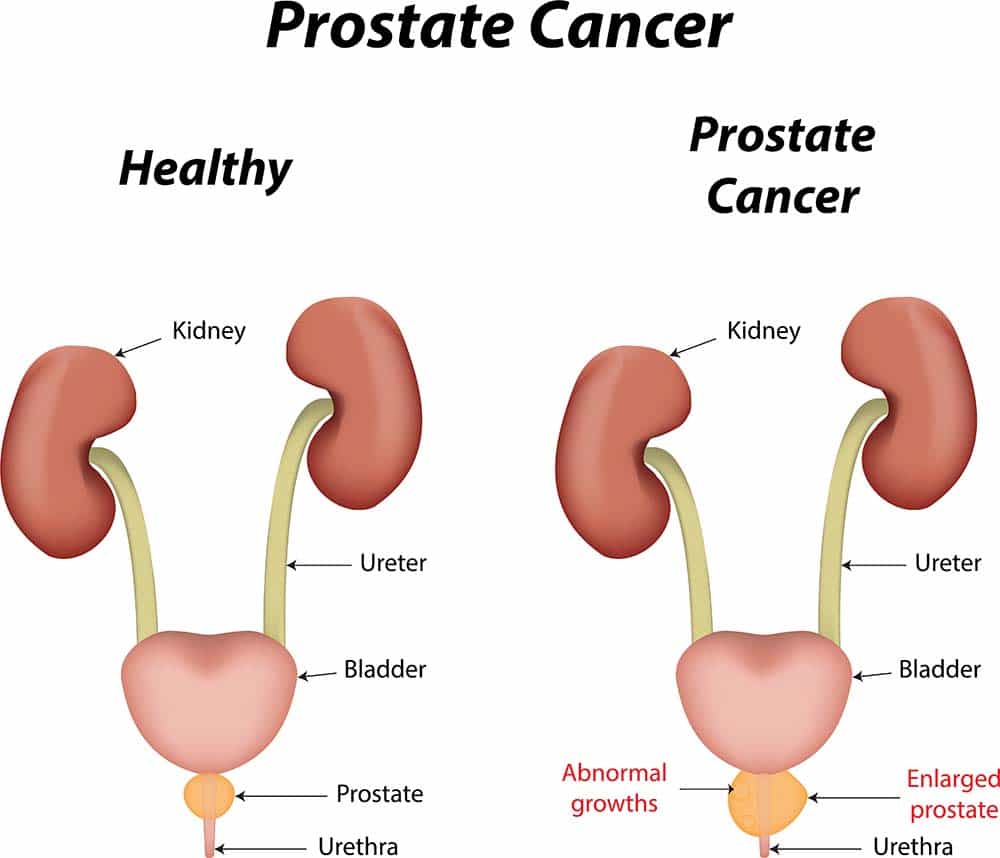
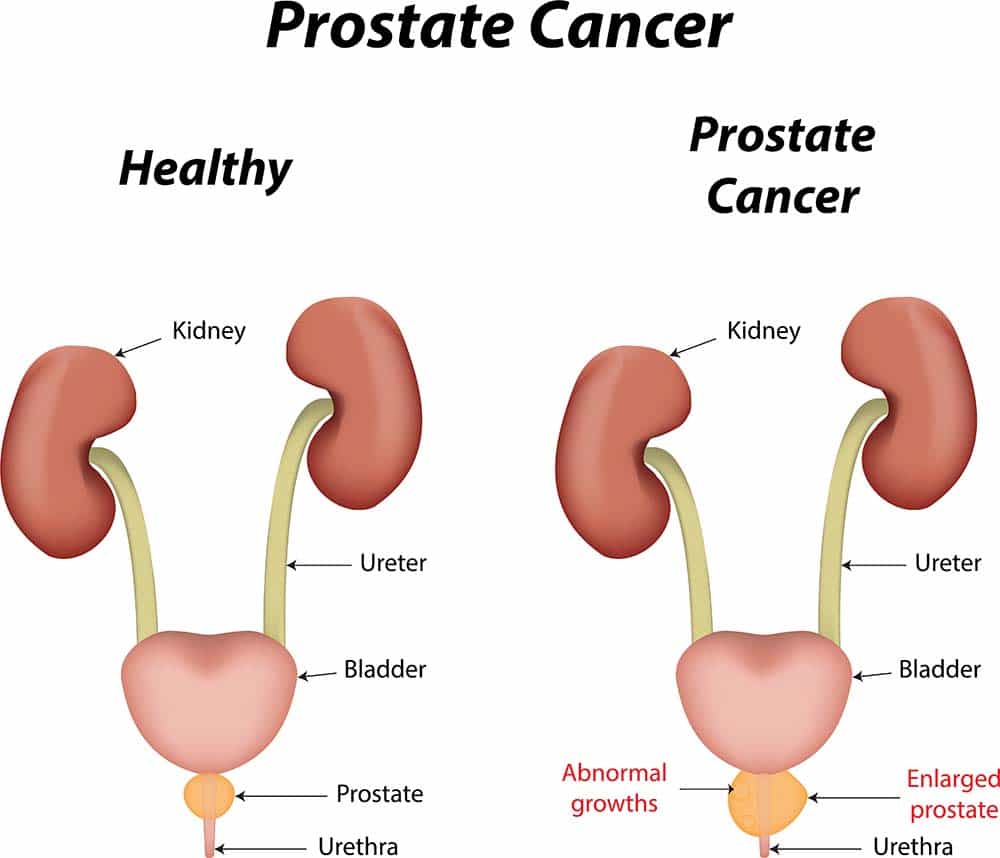
The American Cancer Society estimates there will be 180,890 new cases of prostate cancer and 26,120 deaths from prostate cancer in 2016. This makes prostate cancer the second-most common form of cancer affecting American men, behind skin cancer. It is so common that approximately 1 in 7 American males will be diagnosed with prostate cancer during their lifetime. Thankfully, prostate cancer treatments have come a long way in recent years, which has significantly improved the survival rate for this form of cancer. According to the National Cancer Institute, the death rate from prostate cancer has been declining for more than 20-years — largely as a result of innovative new treatments and better patient awareness. This guide will explain the current Treatment For Prostate Cancer options in the United States.
Treatments For Prostate Cancer
When a person is diagnosed as having prostate cancer, doctors will immediately assess the progression of the illness to determine the best form of treatment. This is performed by taking a prostate cancer biopsy, examining blood PSA levels and performing tests to determine if the patient’s cancer has spread.

They will then consider the patient’s overall health, age and expected life span before deciding which prostate cancer treatment may be appropriate. The doctor will discuss treatment options and their side effects with the patient before agreeing on a treatment plan. In most cases, multiple treatments may be used to tackle the cancer. The following prostate cancer treatments are used in the United States:
Active surveillance or watchful waiting
If a patient’s prostate cancer is diagnosed at an early stage and found to be growing at a slow rate, doctors may decide to delay treatment and simply monitor the cancer’s progress.
This is often done when a physician believes that the side effects of treating the prostate cancer are worse than the symptoms caused by the cancer. Some prostate cancer treatments carry significant side effects including impotence and incontinence.
Active surveillance
Active surveillance describes the monitoring of prostate cancer in individuals with a long life expectancy. If a person is expected to live for another 10, 20 or 30-years, their prostate cancer has plenty of time to grow and become a serious problem. In this situation, physicians may perform tests to monitor the progression of the cancer. This may include:
- PSA test
This is a blood test that is used to detect the presence of prostate cancer. Physicians may perform the test every 3 to 6 months to ensure the prostate cancer is still growing slowly. - Digital rectal exam (DRE)
The physician will perform a DRE at least once a year to check the size of the prostate. - Prostate biopsy
After prostate cancer is discovered the physician may perform regular biopsies to monitor its growth
Additional treatments will be performed if the physician notices the prostate cancer progressing or the patient experiences more serious prostate cancer symptoms.
Watchful Waiting
Because prostate cancer mostly affects older people, many patients have other major health problems that will end their lives before their prostate cancer becomes dangerous. If a patient is already unwell, prostate cancer treatments may cause unnecessary pain and may not improve their life expectancy.
When watchful waiting is used, the doctor will not subject the patient to PSA tests, DREs, or prostate biopsies. They will only take action if the prostate cancer causes serious symptoms like urinary tract blockages or pain.


Surgery
If more action is required, physicians usually turns to surgery in conjunction with radiation therapy. A surgeon will remove the tumor to stop the cancer from spreading any further. The type of surgery that is performed will depend on the progression of the prostate cancer. The surgical options used to treat prostate cancer are:
Radical Prostatectomy
This is the most extreme form of prostate cancer surgery. The prostate, seminal vesicles and some tissue surrounding the prostate are removed from the patient. Access to the prostate is made by performing an incision in the perineum (between the anus and scrotum) or the lower belly. The lymph nodes in the lower belly may also be removed and tested for cancer.
This procedure may interfere with sexual function because the nerves that allow erections and orgasms are located near the prostate. Patients may require additional treatments to restore their sexual function after this procedure. Incontinence is another potential side effect of having this procedure performed.
Robotic or Laparoscopic Prostatectomy
This procedure involves the surgeon making several small incisions in the belly. A laparoscope is inserted into one of the incisions. It is a small surgical instrument that contains a light and camera. Cutting instruments are inserted into the other incisions, then the surgeon uses the laparoscope to find the prostate and remove the tumor.
A robotic-assisted laparoscopic radical prostatectomy involves the use of robotic arms to obtain very precise cuts. All of the tumor is removed during this procedure.
Cryosurgery (Cryotherapy or Cryoablation)
This is a relatively new surgical approach to dealing with prostate cancer. A metal probe is inserted through a small incision to freeze the cancer cells around the prostate. This form of treatment is not an established therapy and researchers do not understand how well it compares to traditional surgical procedures.
Radiation Therapy
Radiation therapy uses high-energy rays to destroy the cancer cells surrounding the prostate. It is performed by a radiation oncologist. Patients will typically receive multiple treatments to ensure that cancer cells surrounding the prostate are killed.
Radiation therapy works by damaging the DNA inside cancer cells, making it impossible for cancer cells to grow or divide.
External-beam Radiation Therapy
The oncologist focusses a beam of x-rays at the area affected by cancer. Sometimes conformal radiation therapy (CRT) is used to precisely locate the tumor that is being targeted, which can reduce damage to healthy tissue surrounding the prostate. This treatment is completely external to the body.
Brachytherapy
Brachytherapy is a form of internal radiation therapy. Radioactive substances are inserted into the prostate, giving off radiation over time which kills the cancer cells surrounding the prostate. The radioactive substances that are inserted into the prostate may be left in for different periods of time, depending on their radioactivity. This form of treatment is often used in conjunction with surgery or other prostate cancer treatments.
Intensity-modulated radiation therapy (IMRT)
IMRT is another form of external beam radiation therapy. A 3-dimensional scan of the prostate is taken to determine the size and location of the tumor. These details are fed into a computer, which calculates the precise levels of radiation that should be applied to kill the cancer cells.
Radium-223
Radium-223 is a radioactive substance that is naturally attracted to areas of high bone turnover within the body. It may be used if prostate cancer has spread from the prostate into the bone surrounding the prostate.
While radiation therapy can be quite effective for treating prostate cancer, there are a number of serious side effects associated with its use. They include fatigue, diarrhea, bleeding from the bowels, incontinence, impotence, and pain.
Proton Therapy (Proton Beam Therapy)
Proton Therapy is an effective type of particle therapy that was first developed in the 1960s. It is similar to external-beam radiation therapy but uses protons instead of x-rays. A proton is a positively charged particle that can destroy cancer cells when pushed into the body at very high speeds. A particle accelerator is used to push the protons towards cancer cells, damaging their DNA. Proton therapy is capable of damaging cancer cells that are deep within the body.
The main advantage of proton therapy is that it can distribute protons very accurately in a three-dimensional pattern — pushing protons into the body at faster speeds to target cancer cells deeper within the body.
Patients will visit a proton therapy center or hospital clinic to have this procedure performed. It is completely pain-free and is completed in a short amount of time.
Androgen deprivation therapy (ADT)
Prostate cancer growth is supported by male sex hormones called Androgens. The most common androgens in men are testosterone, dihydrotestosterone (DHT), and androstenedione.
If there are lower levels of these sex hormones within the body, prostate cancer will not be able to grow as rapidly. These hormones can be lowered by chemically or surgically turning off the function of the testicles (called surgical or chemical castration). Certain drugs can also prevent testosterone from interacting with cancer cells in the body.
ADT to treat prostate cancer at all stages of development, including cancers that have metastasized. It is often used in conjunction with radiation therapy to prevent prostate cancer from reoccurring. The most common forms of androgen deprivation therapies include:
Luteinizing Hormone-releasing Hormone (LHRH) agonists
These medications block messages in the body that tell the testicles to produce more testosterone. They are very effective at reducing the levels of testosterone in the body and the effects of the drug are completely reversible. LHRH agonists are either injected into the skin or inserted beneath the skin.
LHRH antagonist
These drugs, like Abiraterone, stop the body from releasing certain hormones and slow the rate of testosterone production. If your doctor prescribes you Abiraterone, you can get Abiraterone at QuickRx and elsewhere.
Anti-androgens
These drugs stop testosterone in the body from binding with androgen receptors. This prevents testosterone from entering cells within the body — including cancer cells.
Enzalutamide
This is a new type of anti-androgen that blocks signals from androgen receptors in prostate cancer cells. The cancer cells cannot utilize testosterone and their growth rate is dramatically slowed.
Androgen deprivation therapies have a variety of side effects on the male body including weight gain, impotence, depression, loss of muscle mass, and osteoporosis.
Chemotherapy
Chemotherapy uses intravenously injected drugs to kill cancer cells. Most of these drugs either damage the DNA in cancer cells or interfere with chemicals controlling the growth of cancer cells. Chemotherapy is often used if the treating physician believes the cancer has metastasized from the prostate to other parts of the body.
Vaccine Therapy
This treatment creates unique vaccines that boost a person’s immune system and helps it to destroy cancer cells. Blood is taken from the patient and special immune cells are extracted. These cells are modified in a laboratory before being injected back into the patient. The modified immune cells are better at detecting and destroying cancer cells.
Sources
Cancer of the Prostate – SEER Stat Fact Sheets. (2016). Seer.cancer.gov. Retrieved 23 September 2016, from http://seer.cancer.gov/statfacts/html/prost.html
http://www.cancer.org/cancer/prostatecancer/detailedguide/prostate-cancer-key-statistics
What are the key statistics about prostate cancer?. (2016). Cancer.org. Retrieved 23 September 2016, from http://www.cancer.org/cancer/prostatecancer/detailedguide/prostate-cancer-key-statistics




